 The possibility that deep stimulation of the brain could help patients with diabetes regulate their blood sugar was the surprising result of a case where an individual with Obsessive Compulsive Disorder, who was also diabetic and obese, was treated with deep brain stimulation (DBS) for their OCD. By sheer coincidence, their diabetes improved and their blood sugar reduced dramatically.
The possibility that deep stimulation of the brain could help patients with diabetes regulate their blood sugar was the surprising result of a case where an individual with Obsessive Compulsive Disorder, who was also diabetic and obese, was treated with deep brain stimulation (DBS) for their OCD. By sheer coincidence, their diabetes improved and their blood sugar reduced dramatically.
What is Deep Brain Stimulation?
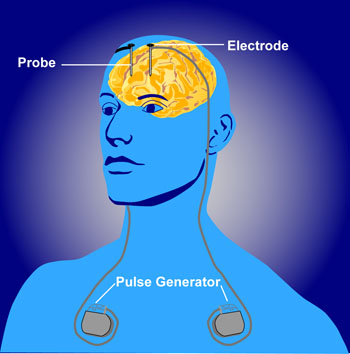
With deep brain stimulation, a device similar to a pacemaker for a heart is implanted into a patient’s body. This device, called a neurostimulator, sends electrical impulses to target locations in the patient’s brain called nuclei. These brain centers are responsible for disorders of movement and have been implicated in neuropsychiatric disorders.
In select brain regions, DBS has been used to treat as diverse conditions as chronic pain, Parkinson’s Disease, dystonia, OCD, and deep clinical depression.
Positioning the Device
The DBS device consists of three parts: an implanted pulse generator (IPG), the lead, and an extension. In most cases, the IPG is placed beneath the collarbone under the skin. Sometimes it is placed in the abdomen. The lead is placed deep into the brain and connected to the IPG via an insulated wire beneath the skin that runs down the side of the neck, behind the ear. The operation may be performed while the patient is awake or under a general anesthetic, depending on the condition being treated.
The placement of the lead into the brain nuclei depends, again, on the condition to be treated. Once implanted, the IPG may be calibrated by a neurologist, technician or a specially trained nurse. The aim of this step is to carefully balance symptom control with minimal side effects.
A Clinical Study
The surprising outcome revealed above led to a purpose-designed clinical study in which 14 people who were not diabetic had already undergone DBS for OCD were recruited. Their DBS stimulators were switched off and their blood sugar was monitored. Researchers discovered that the DBS therapy increased insulin production. They concluded that the treatment increased the insulin sensitivity.
Further experiments using rats showed a relationship between increased dopamine production and higher glucose tolerance. The underlying mechanisms behind this relationship remain to be elucidated, but the results show promise.





